| |
Anti-rheumatic Drugs
|
 |
Rheumatoid arthritis
|
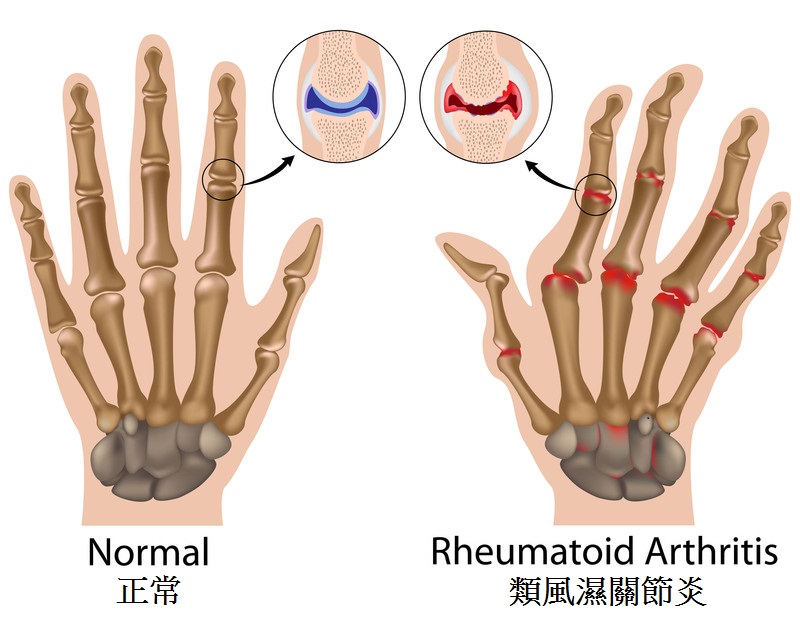
Rheumatoid arthritis is an inflammatory disease that causes pain, swelling, stiffness, and loss of function in the joints. It occurs when the immune system, which normally defends the body from invading external organisms, turns its attack against body’s own tissue synovium (the membrane lining the joints) and causes inflammation. Typical symptoms of rheumatoid arthritis include warmth, redness, swelling, and pain of the synovium.
|
Rheumatic arthritis affects approximately 0.5% to 1% of the adult population in the developed country. It is less prevalent in Hong Kong, with a reported prevalence of 0.35%. Although rheumatoid arthritis can occur at any age, it usually begins after age 40, and is much more common in women. |
As rheumatoid arthritis progresses, the inflamed synovium invades and destroys the cartilage and bone within the joint. The surrounding muscles, ligaments, and tendons that support and stabilize the joint become weak and unable to work normally, leading to pain and joint damage. |
Rheumatoid arthritis typically affects the small joints of the hands and the feet, and usually both sides equally and symmetrically, although any synovial joint can be affected. It is a systemic disease and so can affect the whole body, including the heart, lungs and eyes. |
The severity of rheumatoid arthritis can range from mild to severe which varies greatly between patients. Some people have mild or moderate forms of the disease, with periods of worsening symptoms, called flares. Others have a severe form of the disease that is active most of the time, lasts for many years or a lifetime. Over time, rheumatoid arthritis can cause joints to deform and shift out of place. |
|
|
▲ back to top
Treatment of Rheumatoid arthritis |
 |
There are many ways to treat this disease. The goals of treatment are to relieve pain, reduce inflammation, slow down or stop joint damage, and improve the person’s sense of well-being and ability to function.
|
|
For many years, the approach was to use pain relieve first and waited to prescribe more powerful drugs only if the disease worsen. In recent decades this approach has changed, as studies have shown that early treatment with more powerful drugs—and the use of drug combinations instead of one medication alone—may be more effective in reducing or preventing joint damage. Irreversible joint damage occurs early in the course of disease, thus rapid diagnosis and institution of treatment aimed at preventing progression is crucial.
|
|
|
▲ back to top
Anti-Rheumatic drugs |
|
|
|
Medications used in rhematoid arthritis include: |
 |
| |
|
|
|
1. |
Disease-modifying anti-rheumatic drugs (DMARDs) which are used for slow down the course of the disease.
|
|
e.g.
|
Hydroxychloroquine works by suppress over activity of the immune system and limits inflammation; |
|
|
|
e.g.
|
Methotrexate works by stop or reduce inflammation by altering the body’s defences; |
|
|
|
|
e.g.
|
Sulfasalazine suppress over activity of the immune system in rheumatoid arthritis; |
|
|
|
|
e.g.
|
Leflunomide reduces inflammation by reducing the production of immune cells called ‘lymphocytes’, which are responsible for inflammation; |
|
|
|
|
e.g.
|
Azathioprine helps to suppress over activity in the immune system. This helps to reduce pain and swelling by limiting inflammation; |
|
|
|
|
e.g. |
Cyclosporin A (Ciclosporin) helps to suppress over activity in the immune system. This helps to reduce pain and swelling by limiting inflammation. |
|
|
|
|
2. |
Biologic DMARDs, these are genetically engineered medications that help reduce inflammation and structural damage to the joints by interrupting the cascade of events that drive inflammation. These may be used in people with more serious disease.
|
|
|
|
|
e.g.
|
Tumour necrosis factor alpha (TNFα) blocker (e.g. etanercept, infliximab, adalimumab). TNFα is a cytokines, substances released by the body during inflammation. TNFα blocker is a protein that has been designed to block the activity of a chemical messenger - tumour necrosis factor (TNF). By blocking TNF, it reduces the inflammation and other symptoms of the diseases; |
|
|
|
|
e.g.
|
Interleukin 6 (IL-6) inhibitor (e.g. tocilizumab). Tocilizumab is a monoclonal antibody. Tocilizumab has been designed to attach to the receptor for a messenger molecule or ‘cytokine’ in the body called interleukin-6. This messenger is involved in causing inflammation and is found at high levels in patients with rheumatoid arthritis. By preventing interleukin-6 attaching to its receptors, tocilizumab reduces the inflammation and other symptoms of this disease; |
|
|
|
|
e.g.
|
Co-stimulation blocker (e.g. abatacept). Abatacept is a protein that has been designed to suppress the activity of ‘T cells’, immune system cells that are involved in causing the inflammation in rheumatoid arthritis; |
|
|
|
|
e.g. |
Rituximab decreases the number of B-cell lymphocytes, one of the white blood cells responsible for causing inflammation and for fighting infection. In rheumatoid arthritis, rituximab (a monoclonal antibody) attaches to the surface antigen (CD20) of the B lymphocytes in the joints; leads to the death of the B lymphocytes and reduce inflammation. |
|
|
|
|
3. |
Janus kinase inhibitor (e.g. tofacitinib). It is an immunosuppressant (a medicine that reduces the activity of the immune system) that works by blocking the action of enzymes known as Janus kinases. These enzymes play an important role in the process of inflammation and damage of the joints that occurs in rheumatoid arthritis. By blocking the enzymes, tofacitinib is expected to reduce the inflammation and other symptoms of the disease. |
|
|
4. |
Corticosteroids (e.g. prednisolone) are used for managing flares with recent onset or established disease to rapidly decrease inflammation. For more information on oral corticosteroids, please refer to
|
|
http://www.drugoffice.gov.hk/eps/do/en/consumer/news_informations/dm_02.html
|
|
|
|
5. |
Analgesics (e.g. paracetamol, codeine and combination preparations) and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) (e.g. naproxen and diclofenac) including Cyclo-OXygenase-2 (COX-2) inhibitors (e.g. celecoxib and etoricoxib) are used for pain control and reduce inflammation. For more information on analgesics and NSAIDs, please refer to respective links.
|
|
http://www.drugoffice.gov.hk/eps/do/en/consumer/news_informations/dm_16.html |
|
http://www.drugoffice.gov.hk/eps/do/en/consumer/news_informations/dm_03.html
|
|
|
|
|
All the above named medicaions are registered in Hong Kong, most of them are available in oral dosage form, some medications (e.g. biological DMARDs) are available in injection / infusion dosage forms only. DMARDs, Janus kinase inhibitor, corticosteroids, the majority of NSAIDs, and codeine containing analgesics are prescription only medicine, while paracetamol is over the counter medicine.
|
|
|
▲ back to top
Common side effects and precautions
Anti-rheumatic drugs
|
Common side effects
|
Precautions
|
Disease-modifying anti-rheumatic drugs (DMARDs) |
| 1. Hydroxychloroquine |
Gastro-intestinal disturbances, headache and skin reactions (rashes, pruritus).
|
- Should not be used in patient with a history of hypersensitivity to hydroxychloroquine or other similar medicines.
- Should not be used in patients with eye problem which affects the retina, inside of eye or change in eye colour.
- Avoid in pregnancy or breastfeeding.
- Use with caution in patient with moderate to severe hepatic impairment.
- Seek medical advice if the following is observed:
eye problems, muscle weakness, severe skin reaction, sign of liver problems (yellowing of eye / skin) or lowering of blood glucose level.
|
| 2. Methotrexate |
Mucositis, swelling of the mouth, nausea and vomiting/ abdominal distress, anorexia (eating disorder), bone-marrow suppression (leucopenia), liver damage, raised liver enzymes, renal failure,
pulmonary reaction (e.g. persistent cough or develop shortness of breath), headache, dizziness, fatigue,
loose stools,
a skin rash with reddening of the skin.
|
- Should not be used in active infection and immunodeficiency syndromes.
- Avoid in hepatic impairment, renal impairment, severe blood problems, pregnancy or breastfeeding.
- Avoid antibiotics which prevent the production of folic acid (e.g. Co-trimoxazole).
- Seek medical advice if the following is observed: Severe skin rash that causes blistering, persistent cough, pain or difficulty breathing or become breathless (maybe caused by fluid in lung), skin rash and fever with swollen glands (hypersensitivity reaction), signs of infection.
|
| 3. Sulfasalazine |
Indigestion, heartburn, nausea (feeling sick),
cough,
difficulty sleeping,
dizziness, fever,
blood disorder, protein in urine, ringing in the ears, stomatitis (inflamed mouth), changes in taste and itchy skin.
|
- Avoid in severe renal impairment.
- Use with caution in patient with porphyria (a rare blood pigment disorder), asthma, deficiency of enzyme known as glucose-6-dehydrogenase, hepatic impairment, renal impairment.
- Use with caution in pregnancy or breastfeeding.
- Should not be used in patient with history of allergic to salicylates, or sulfonamides.
- Seek medical advice if severe skin rash that causes blistering or peeling of skin develops.
|
| 4. Leflunomide |
Leucopenia (decrease in the number of white blood cells), mild allergic reaction, increased creatine phosphokinase levels (a marker of muscle damage), paraesthesia (abnormal skin sensations like tingling), headache, dizziness, increased blood pressure, diarrhoea, nausea, vomiting,
anorexia, oral mucosal disorders, abdominal pain,
increase liver enzyme levels, hair loss, rash,
dry skin, pruritus (itching),
tenosynovitis (inflammation of tendon and its sheath), loss of appetite, weight loss and asthenia (weakness).
|
- Should not be used in patient with immunodeficiency, severe hypoproteinaemia, serious infection, or bone marrow problem.
- Avoid in hepatic impairment, moderate or severe renal impairment, pregnancy or breastfeeding.
- Seek medical advice if the following is observed: sign of allergic reaction, severe skin reaction, develop symptoms of pancytopenia (e.g. pale skin, tiredness, or bruising), sign of liver problem (yellow discolouration of eyes or skin), symptoms of an infection, sign of lung disease (difficulty in breathing), or peripheral neuropathy (tingling or pain).
|
| 5. Azathioprine |
Infections, reduction in bone marrow function, low white blood cell level (may cause an infection), low blood platelet level (may cause you to bruise or bleed easily).
|
- Must not be used in people who are hypersensitive (allergic) to azathioprine, mercaptopurine or any of the other ingredients in the product.
- Avoid in pregnancy or breastfeeding.
- Tell your doctor if you have liver or kidney disease, ‘Lesch-Nyhan Syndrome’, have a condition where your body produces too little of something called TPMT or ‘thiopurine methyltransferase’, have ever suffered from chickenpox or shingles, going to have a vaccination.
- While taking Azathioprine, take care to avoid too much sun, cover up and use sunscreen.
|
| 6. | Cyclosporin A (ciclosporin) |
|
Kidney problems, high blood pressure, headache, shaking of your body which you cannot control, excessive growth of body and facial hair, high level of lipids in your blood.
Fits (seizures), liver problems, high level of sugar in your blood, tiredness, loss of appetite, nausea (feeling sick), vomiting, abdominal pain, constipation, diarrhoea, acne, hot flushes, fever, low level of white blood cells, feeling numb or tingling, pain in your muscles, muscle spasm, stomach ulcer, gum tissue overgrowing and covering your teeth, high level of uric acid or potassium in your blood, low levels of magnesium in blood.
|
- Must not be used in people who are hypersensitive (allergic) to cyclosporin A or any of the other ingredients of the product, products containing Hypericum perforatum (St John´s Wort), or products containing dabigatran etexilate (used to avoid blood clots after surgery) or bosentan and aliskiren (used to reduce high blood pressure).
- Avoid in pregnancy or breastfeeding.
- Do not use in patients with kidney problems (except for nephrotic syndrome), have infection which is not under control with medication, have any type of cancer, have high blood pressure (hypertension) which is not under control with medication.
|
Biologic DMARDs |
| 7. | Etanercept, Infliximab, Adalimumab |
|
Infections (including colds, sinusitis, bronchitis, urinary tract infections and skin infections), injection site reactions (including bleeding, bruising, redness, itching, pain, and swelling), allergic reactions, fever, itching, antibodies directed against normal tissue (autoantibody formation).
|
- Should not be used in active infection e.g. tuberculosis (TB), hepatitis B (Hep B), other serious infection such as pneumonia or sepsis (serious bacterial infection of the blood), or severe heart failure (infliximab).
- Avoid in pregnancy or breastfeeding.
- Use with caution in hepatic impairment (etanercept).
- Tell your doctor if you have recurrent infection or history of TB, Hep B, have heart failure, blood disorder, lung disease (e.g. Chronic Obstructive Pulmonary Disease) or have or have had cancer, have recently received or are scheduled to receive a vaccine; have diabetes or an immune system problem.
- Seek medical advice if you develop signs of serious infection, serious allergic reaction, blood disorder, nerve disorders, worsening of heart failure.
|
| 8. Tocilizumab |
Upper respiratory tract infections (colds), nasopharyngitis (inflammation of the nose and throat), headache, hypertension (high blood pressure) and abnormal liver function tests,
high blood fat (cholesterol) levels. Stomach (abdominal) pain, mouth ulcer, gastritis, dizziness, peripheral oedema, antibody formation, hypersensitivity,
low white blood cell counts (leucopenia, neutropenia). The most serious side effects are serious infections, complications of diverticulitis (inflammation of the gut) and hypersensitivity (allergic) reactions.
|
- Must not be used in patients who have an active, severe infection.
- Avoid in pregnancy and breastfeeding.
- Seek medical advice if you have the following condition: any kind of infection, short- or long-term, or if you often get infections, have had tuberculosis, have had intestinal ulcers or diverticulitis, have liver disease, have been recently vaccinated, or are planning a vaccination, have cancer, have cardiovascular risk factors such as raised blood pressure and raised cholesterol levels, have moderate to severe kidney function problems, have persistent headaches.
|
| 9. Abatacept |
Infection, abdominal pain, diarrhoea, dyspepsia, nausea, vomiting, stomatitis, flushing, hypertension, cough, dizziness, fatigue, headache, paraesthesia (abnormal skin sensations like tingling), leucopenia (decrease in the number of white blood cells), pain in extremities and conjunctivitis.
|
- Must not be used in patients who are hypersensitive (allergic) to abatacept or any of the other ingredients.
- Must not be used in patients with severe and uncontrolled infections, such as sepsis (when bacteria and their toxins circulate in the blood and start to damage the organs) or ‘opportunistic’ infections (infection caused by usually harmless micro-organism in patient with weakened immunity).
- Avoid in pregnancy and breastfeeding.
- Seek medical advice if you have the following condition: history of tuberculosis, have viral hepatitis, have cancer, have recently received or are scheduled to receive a vaccine, develop signs of allergic reaction, any kind of infection / symptoms of infection.
|
| 10. Rituximab |
Infections such as pneumonia, urinary tract infection, reaction related to infusion, changes in blood pressure, nausea, rash, fever, feeling itchy, runny or blocked nose and sneezing, shaking, rapid heartbeat, and tiredness, headache.
|
- Should not be used in patient with severe infection or weak immune system.
- Avoid in pregnancy or breastfeeding.
- Use with caution in patients receiving cardiotoxic chemotherapy, with history of cardiovascular disease or have hepatitis.
- Seek medical advice if you develop sign of infection (including fever, cough or sore throat), memory loss, trouble thinking, difficulty in walking or sight loss (maybe caused by serious brain infection).
|
Janus kinase inhibitor |
| 11. Tofacitinib |
Upper respiratory tract infections (common cold, sinus infections) headache, diarrhoea, nasal congestion, sore throat and runny nose.
|
- Must not be used in patients who are hypersensitive (allergic) to tofacitinib or any of the other ingredients in the product.
- Do not use in patients with severe liver problems.
- Avoid in patients with active, including localised, infections.
- Used with caution in those with chronic or recurrent infection, exposure to tuberculosis, a history of serious or opportunistic infection, or underlying conditions that may predispose to infection.
- Used with caution in patients with an increased risk, such as those with a history of diverticulitis (inflammation in parts of the large intestine) or ulcers in stomach or intestines.
- Used with caution in patients with a known malignancy.
- Avoid in pregnancy or breastfeeding.
- Seek medical advice if you have diabetes, HIV/AIDS or a weak immune system, recently been vaccinated or plan to get vaccinated, liver or kidney problems including kidney transplant surgery, chest pain or any heart problems, lung disease or shortness of breath, high cholesterol, plan to have surgery or a medical procedure.
|
|
|
▲ back to top
General advice
|
|
 |
- Rest when you’re tired. Rheumatoid arthritis can make you prone to fatigue and muscle weakness. People with rheumatoid arthritis need a good balance between rest and exercise, with more rest when the disease is active and more exercise when it is not. Rest helps to reduce active joint inflammation and pain and to fight fatigue.
- Gentle exercise can help strengthen the muscles around your joints, and it can help fight fatigue you might feel. Exercise can also help people sleep well and manage weight.
|
|
|
|
- Heat can help ease your pain and relax tense, painful muscles. Cold may dull the sensation of pain. Cold also has a numbing effect and decreases muscle spasms.
|
| |
- Find way to cope with pain by reducing stress in your life. People with rheumatoid arthritis face emotional challenges as well as physical ones. Stress also may affect the amount of pain a person feels. There are a number of successful techniques for coping with stress. Regular rest periods can help, as can relaxation, distraction, or visualization exercises.
|
| |
- Healthy diet: an overall nutritious diet with enough—but not an excess of—calories, protein, and calcium is important. Patients taking anti-rheumatic drugs need to be careful about drinking alcoholic. Those taking methotrexate need to avoid alcohol altogether because one of the most serious long-term side effects of methotrexate is liver damage.
|
|
|
|
▲ back to top
Communication with your doctor
|
|
 |
|
- Inform your doctor of your medical history, as some diseases may warrant special precautionary measures.
- Inform your doctor that you are pregnant (plan to become pregnant) or breast feeding as some of the anti-rheumatic drugs should not be taken by women who are pregnant or breast feeding.
|
|
- Seek medical advice immediately if you experience any symptoms or side effects suspected to be related to anti-rheumatic drugs. Your doctor may review your type of medication.
- Have regular medical follow-ups as advised by your doctor.
|
|
|
|
▲ back to top
Storage of anti-rheumatic drugs
Anti-rheumatic drugs should be stored according to condition specified on the label, for oral drug usually kept in a cool and dry place, whereas for biological DMARDs usually store at 2-8°C. Furthermore, drugs should be kept properly in places unreachable by children to prevent accidental ingestion.
|
|
▲ back to top
|
|
Acknowledgement: The Drug Office would like to thank the Professional Development and Quality Assurance (PD&QA) for their valuable contribution to the preparation of this article.
|
|
|
|
|


